Understanding Hemorrhagic Disorders: Causes, Classification, and Implications
Introduction
Hemorrhagic disorders encompass a broad spectrum of medical conditions characterized by excessive bleeding, either externally or internally. These disorders can significantly impact health and require prompt diagnosis and intervention. Understanding the underlying causes and the classification of hemorrhagic disorders is crucial for effective management and treatment. This article aims to provide a comprehensive overview of the various causes of hemorrhagic disorders, their classification, and the implications for patient care.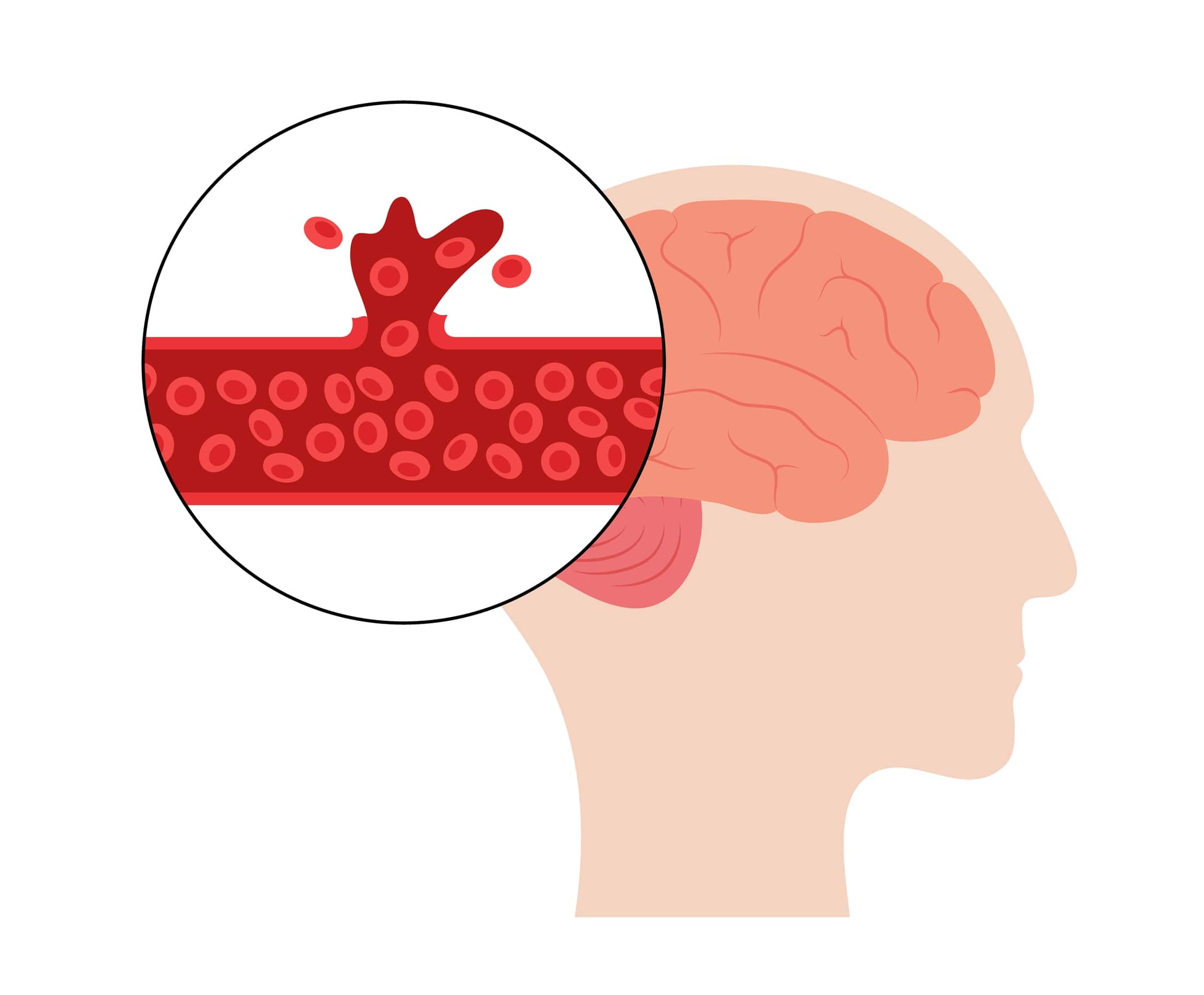
Overview of Hemorrhagic Disorders
Hemorrhagic disorders can arise from a multitude of factors, ranging from genetic abnormalities to acquired conditions. The resultant bleeding may occur due to disruptions in the coagulation cascade, vascular integrity, or platelet function. It is vital for healthcare professionals to identify the specific type of hemorrhagic disorder a patient may have to initiate appropriate treatment.
Classification of Hemorrhagic Disorders
Hemorrhagic disorders can be broadly classified into two main categories: primary disorders and secondary disorders. Each category is further divided based on the underlying mechanisms of bleeding.
1. Primary Hemorrhagic Disorders
Primary hemorrhagic disorders are often genetic or inherited conditions that affect the body’s ability to coagulate blood effectively. These include:
- Hemophilia: This is an X-linked recessive disorder, most commonly affecting males. Hemophilia A results from a deficiency of Factor VIII, while Hemophilia B is due to a deficiency of Factor IX. Patients with hemophilia experience spontaneous bleeding episodes, particularly into joints and muscles.
- Von Willebrand Disease (vWD): This is the most common inherited bleeding disorder. It is caused by a deficiency or dysfunction of von Willebrand factor, which is essential for platelet adhesion. Patients often present with easy bruising and mucosal bleeding.
- Platelet Disorders: Conditions such as Glanzmann thrombasthenia and Bernard-Soulier syndrome affect platelet function and aggregation. These conditions can lead to prolonged bleeding times and increased susceptibility to hemorrhage.
- Congenital Fibrinogen Deficiency: This rare disorder involves a deficiency of fibrinogen, a key protein in the clotting process, resulting in severe bleeding episodes.
2. Secondary Hemorrhagic Disorders
Secondary hemorrhagic disorders are acquired conditions that can develop due to various factors, including medications, disease processes, and environmental influences. The key subtypes include:
- Acquired Coagulation Disorders: Conditions such as liver disease, vitamin K deficiency, and disseminated intravascular coagulation (DIC) can impair the coagulation cascade. In liver disease, for instance, the production of clotting factors is reduced, leading to an increased risk of bleeding.
- Thrombocytopenia: A reduction in platelet count can occur due to bone marrow disorders, autoimmune diseases (such as immune thrombocytopenic purpura), or the effects of certain medications. This condition can significantly heighten the risk of hemorrhagic events.
- Medications: Anticoagulants, such as warfarin and direct oral anticoagulants (DOACs), can lead to excessive bleeding if not monitored properly. Additionally, antiplatelet medications (e.g., aspirin) can increase bleeding risk, especially in patients undergoing surgical procedures.
- Vascular Disorders: Conditions such as vasculitis, which causes inflammation of blood vessels, can lead to bleeding due to vessel damage. Additionally, conditions like aneurysms can result in catastrophic hemorrhagic events when ruptured.
Causes of Hemorrhagic Disorders
Understanding the specific causes of hemorrhagic disorders is essential for effective diagnosis and management. The following are key factors contributing to these conditions:
Genetic Factors
Many hemorrhagic disorders are genetically inherited. Mutations in genes responsible for clotting factor production or platelet function can lead to various bleeding disorders. For instance, mutations in the F8 gene lead to Hemophilia A, while mutations in the VWF gene are associated with von Willebrand Disease.
Acquired Conditions
Acquired conditions can significantly impact hemostasis, leading to hemorrhagic disorders. Liver disease, for example, affects the production of clotting factors and may result in coagulopathy. Similarly, vitamin K deficiency, often seen in malnutrition or certain malabsorption syndromes, can lead to reduced levels of clotting factors II, VII, IX, and X.
Environmental Factors
Certain environmental factors can exacerbate or trigger hemorrhagic disorders. For example, individuals with genetic predispositions may experience bleeding episodes following surgery, trauma, or infections. Additionally, the use of anticoagulant medications, either therapeutically or as a result of medical management, can precipitate bleeding in susceptible individuals.
Implications for Patient Care
The management of hemorrhagic disorders requires a multidisciplinary approach, including diagnosis, treatment, and ongoing monitoring. Clinicians must be vigilant in recognizing signs of bleeding and performing appropriate laboratory tests to identify the underlying cause.
Diagnosis
Diagnosis often involves a combination of patient history, physical examination, and laboratory testing. Key tests may include:
- Complete Blood Count (CBC): This test can identify thrombocytopenia and assess hemoglobin levels.
- Coagulation Studies: Prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time can help evaluate the coagulation cascade.
- Platelet Function Tests: Assessing platelet aggregation can help diagnose specific platelet disorders.
Treatment
Treatment strategies vary based on the type of hemorrhagic disorder and its underlying cause. Key interventions may include:
- Replacement Therapy: In conditions like Hemophilia, replacement therapy with clotting factors can be lifesaving.
- Desmopressin: This medication can be used in patients with von Willebrand Disease to increase levels of von Willebrand factor and factor VIII.
- Antifibrinolytics: Medications like tranexamic acid may be employed to help stabilize clots and reduce bleeding.
- Transfusions: In cases of severe hemorrhage, platelet or blood transfusions may be necessary to restore hemostasis.
Monitoring and Follow-Up
Patients with hemorrhagic disorders require ongoing monitoring to assess treatment efficacy and adjust therapies as necessary. Regular follow-up visits, along with periodic laboratory evaluations, can help ensure optimal patient outcomes.
Conclusion
Hemorrhagic disorders present significant challenges in clinical practice, requiring a comprehensive understanding of their causes and classifications. By recognizing the various types of hemorrhagic disorders and their underlying mechanisms, healthcare professionals can implement appropriate diagnostic and treatment strategies to improve patient outcomes. As research advances, the development of novel therapies and enhanced diagnostic techniques holds promise for better management of these complex conditions, ultimately leading to improved quality of life for affected individuals. Understanding and addressing the multifactorial nature of hemorrhagic disorders is essential for optimizing patient care and reducing the burden of excessive bleeding.
References
- Franchini, M., & Mannucci, P. M. (2013). Hemophilia and von Willebrand disease: a historical perspective. Blood Transfusion, 11(3), 392-395.
- Srivastava, A., et al. (2013). Guidelines for the Management of Hemophilia. Haemophilia, 19(1), e1-e47.
- Kessler, C. M. (2008). Hemophilia: A comprehensive approach to its management. Hematology/Oncology Clinics of North America, 22(5), 953-965.
- Mannucci, P. M. (2016). The history of hemophilia. Blood Transfusion, 14(1), 8-12.
